LAFAYETTE, Ind. — "I'm the lucky one here. I know that," said Dave Knott.
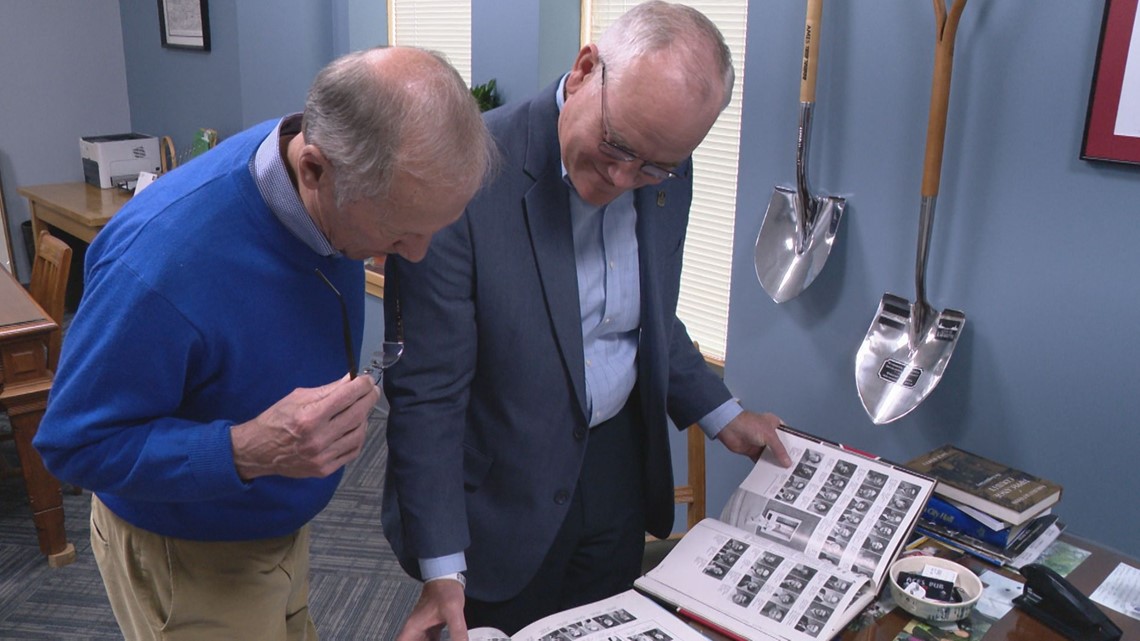
Forty years have come and gone since Knott first met Tom Murtaugh, teaching him at Lafayette Jefferson High School.
"Honors algebra, geometry and economics," Murtaugh said, counting off the years he had Knott as a teacher in school.
"OK," Knott said. "So that would have been three years."
The pair flipped through old yearbooks from 1982 and 1983, the photos stirring up old memories.
"When I was in high school, I had Mr. Knott, as I called him at that time, for both mathematics and economics. He was a phenomenal teacher and obviously left an impression," Murtaugh said. “He truly is an icon in this community. I mean, he had very successful teams as a football coach and he obviously taught a lot of people and left impressions on a lot of people in this community. People know him, people remember him."

After graduating high school, Murtaugh and Knott stayed in touch, bumping into one another around Lafayette and catching up at the YMCA from time to time.
But in the fall of 2018, as Knott dealt with kidney disease that left him sick, spending hours in dialysis daily and waiting for a second kidney transplant, his daughter made a post to social media in hopes of finding her dad a donor.
"That post talked about his need for a kidney," Murtaugh said. "And it just kind of hit me and it's like you know, I'm healthy, I could do this."
Call it fate or Facebook, Murtaugh immediately jumped in to start the testing with IU Health. But he didn't tell Knott, not for months until he could be sure he was able to be a match for his former teacher.


"At that point in time, I had undergone five months of dialysis, which is just awful. And I was debating, is this going to be the rest of my life where I have to do this? And he saved my life," Knott said.
Families waited anxiously as the doctors at IU Health University Hospital started the transplant on March 29, 2019.
"I had some nerves, but I knew I was doing the right thing," Murtaugh said. "And Barb would text me every once in a while before the surgery and say, 'You're not getting nervous, are you? You're not going to change your mind?' And I said, 'No, I'm not going to change my mind.'"
"I thought, 'Hurry up and send that gurney down here so we can get going,' because I knew I was going to feel better," Knott said.
Within two days of the transplant, Knott said his kidney's creatinine levels went from nearly fatal to nearly normal. For Murtaugh, his gift of his kidney has also given him a second family.
"We've tried to make Tom a part of our family, my kids are all somehow connected to Tom and my wife certainly is. I guess I thank him every day. I thank him as often as I can, but it's never going to be enough, I can't do enough to thank him for what he did," Knott said.
"And it is just great to see that he has his life back, that he's able to do everything he wants to do and his family is able to enjoy his company and it's just, it's touching," Murtaugh said.
Now, nearly three years later, Knott said not a day goes by that he doesn't think about the surgery and of Tom Murtaugh, grateful for the gift of life from his former student.
"He's the hero here," Knott said. "I'm just the participant."
For more information about IU Health's kidney donation program including how to find out if you could provide a lifesaving match for someone, click here.
Becoming a donor
Dr. Asif Sharfuddin, a nephrology and kidney diseases specialist at IU Health explains the process for how those interested in donating works.
"Once an individual submits their information online to be considered as a potential living donor, a health screen is completed to make sure they are a suitable candidate. Donor safety is our priority, and our team works to ensure this and provide support throughout the donation process," Sharfuddin said in a statement to 13News. "Before testing begins, potential donors are educated about their rights and the potential risks of living donation. Blood type matching and tissue type (HLA matching) testing between the recipient and potential donor are required. The potential donor will undergo a careful and thorough evaluation process which includes multiple tests and consultations to determine if they are eligible for donation."
13News asked Sharfuddin about the living donor process.
"If the candidate’s blood type is not compatible with the intended kidney recipient, there may still be options for living donation through paired donation, also known as a donor swap, which matches incompatible recipient/donor pairs with other incompatible pairs. IU Health routinely performs such exchange transplants and these typically make up around 15-20% of our living donor transplants," he said. "If approved to donate, a surgery date is scheduled that works for the donor and recipient. The entire process from start to end for becoming an approved donor generally takes 2 to 3 months."
How challenging is it to find a living donor willing to donate a kidney or other organ?
"It could be a challenge to find a living donor, as many people are not suitable to donate due to existing medical conditions such as obesity, heart disease, advanced diabetes, hypertension or issues and so on. Some patients can modify some of their risks by losing weight to become successful donors," Sharfuddin said. "Finding a donor with a matching blood type can also be a challenge, but with the Kidney Paired Exchange option, that is generally not a barrier to organ donation.
"It is advantageous to look for as many potential living donors as possible, which increases the odds that an individual will likely qualify to be a direct donor or an exchange (swap) donor. Therefore, looking broadly for a donor is important. We understand it is hard for someone in need of an organ donation to ask for this kind of gift. IU Health provides resources on helping family find ways to be a living donor champion."
Are more living donors needed to consider donating?
"It continues to be very important to bring awareness about how people can provide the life-saving gift of a kidney through living donation. There are currently more than 90,000 people in the country waiting for a kidney transplant. In 2021, around 19,000 received a transplant, of which approximately 5,900 of those were living donor transplants," Sharfuddin said. "In Indiana, there are currently 961 patients waiting for a kidney transplant. In 2021, a total of 289 kidney-alone transplants were done, of which there were only 62 living donor transplants done in 2021.
"The longer a patient waits for a transplant in the state of kidney failure, the worse their outcomes will be, and many patients (approximately 15-20%) may not end up receiving a transplant as other cardiovascular complications set in which makes the patient too sick to receive a transplant," he continued. "Living donation can shorten waiting times for those waiting for a kidney and ultimately save the lives of others by curing their kidney failure."
How important are living donors when it comes to organ donation?
"Waiting times for a kidney from a deceased donor can be quite long, varying from 2 to 6 years. Some patients are not able to wait that long and end up with other complications of kidney failure," Sharfuddin said. "A kidney from a living donor can function better and last longer because the donor is healthy. It also functions better because the kidney is transplanted into the recipient shortly after being removed from the donor. Because of these factors, patients receiving a kidney from a living donor often have better outcomes than patients receiving a kidney from a deceased donor. This advantage continues long term.
"Every living donor transplant that takes place allows one more deceased donor option to be accessible to those patients who don’t have any living donors for themselves, therefore helping individuals in kidney failure waiting on the transplant list."
What are some of the reasons people may need a kidney transplant? How serious must their conditions be to be placed on a transplant list?
"The most common causes of kidney failure in the U.S. is diabetes, hypertension or a combination of both. Other conditions such as polycystic disease (PKD), and other autoimmune conditions such as IGA nephropathy, FSGS, lupus are common reasons for kidney failure needing transplants.
"Any patient who is in kidney failure (dialysis or have a kidney function below 20%) whichever comes first, is eligible to listed to receive a transplant, provided they are medically suitable candidate and the benefits of a transplant outweigh the risks of a transplant," Sharfuddin said. "Severity of kidney failure is not a factor in listing."
What is IU Health's role when it comes to kidney transplants and other transplants around the state of Indiana?
"IU Health is the largest kidney transplant program in the state and is one of the leading programs in the country. Of the 250 transplant centers in the U.S. in 2021, IU Health ranks No. 18 in kidney transplant volume. IU Health also is the only center in the state which offers multi-organ transplants for patients needing pancreas or liver transplants with kidney transplants. We also engaged in the National Kidney Paired Exchange Program for patients who have an incompatible living donor," Sharfuddin said. "In addition, IU Health offers transplantation for various high-risk conditions such as HIV, advanced cardiovascular issues, prior bone marrow malignancies, or multiple myeloma. We are privileged to be able to help many high-risk patients who are in need a transplant."
How much of a difference can a kidney or other organ transplant make for patients in need who come through IU Health?
"It is a positive life-changing and life-saving event for any person to receive a kidney transplant or other organ transplants such as a pancreas, liver, intestine, heart or lung. Our large, dedicated multidisciplinary team, including experienced transplant nurses, coordinators, surgeons and physicians evaluate every possible candidate who needs an organ transplant," Sharfuddin said. "With access to advanced and cutting-edge therapies, in combination with the IU School of Medicine, we strive to transplant those patients who otherwise may not be considered at some other medical centers in the country."