GREENWOOD, Ind. (WTHR) — Greenwood resident Bryan Hussung, 44, just returned home after spending 14 days in the hospital dealing with the coronavirus.
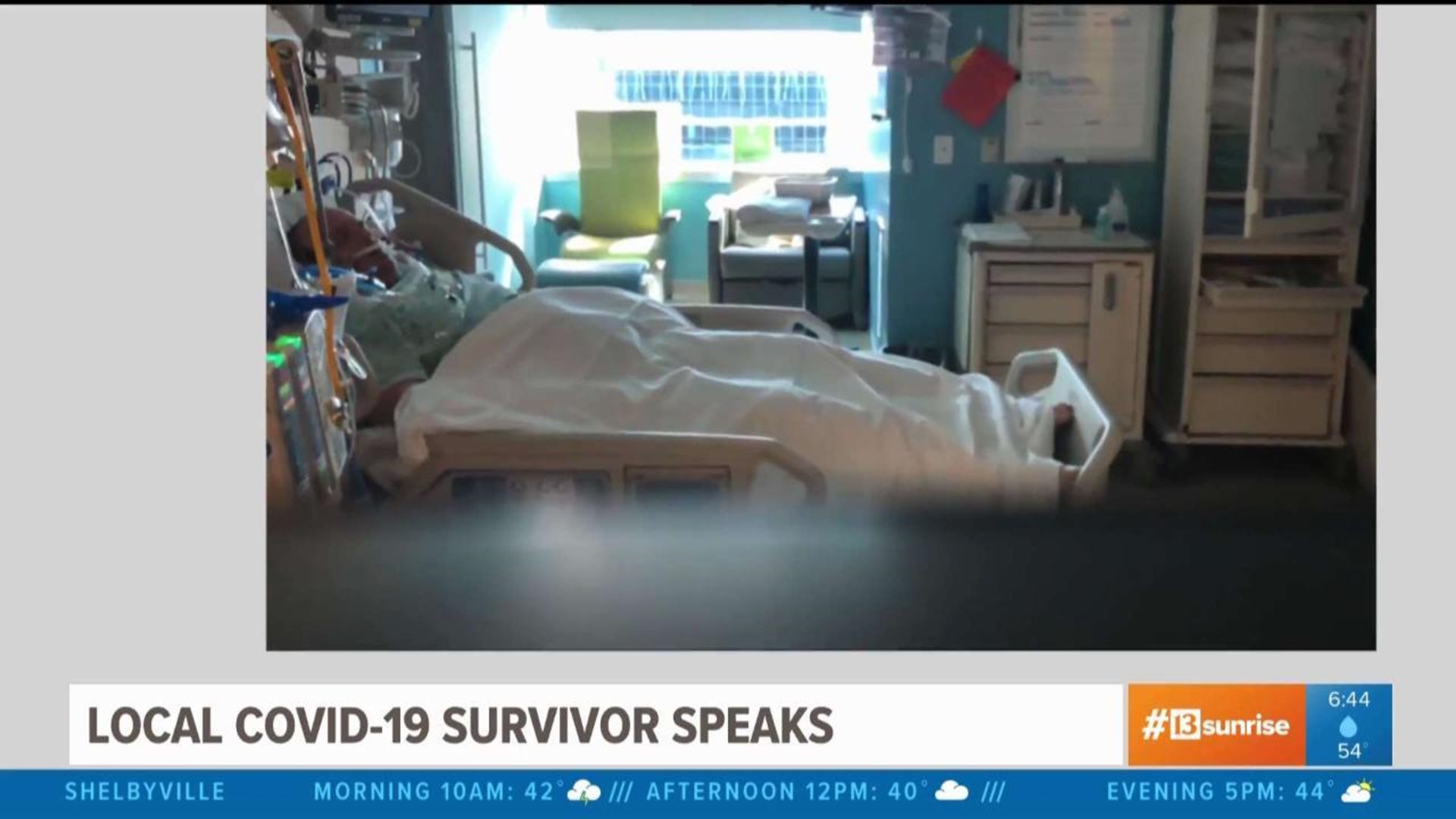
Bryan was at Eskenazi Hospital for 13 of those days and on a ventilator for 10 days. Bryan said within 24 hours of walking into the hospital, he was on that ventilator.
Bryan's wife Jennifer said he had a pre-existing condition with exercise-induced asthma, but the doctors didn't say it necessarily caused him to become ill so quickly.
When he finally came home last week, everyone in the Hussungs' neighborhood made signs, blew up balloons, spun noisemakers and welcomed Bryan home with a social distancing parade.
As part of our "Facts Not Fear" initiative, we are providing the entire 25-minute FaceTime transcript between 13News' Carlos Diaz and the Hussungs.
___
Carlos Diaz: "I'm so happy to be FaceTiming with you because you are a survivor! Tell me about how this started."
Bryan Hussung: "Well, it actually just started as maybe some sinus symptoms, maybe flu-like symptoms. And it turned. Quick. Almost within hours."
CD: "So did you feel you had the flu for a few days and then all of a sudden it got bad really quickly?"
BH: "Yeah, that's pretty much how I felt. Temperature just didn't kind of feel good, kind of sluggish. Now wasn't the corona symptoms like what like we were thinking, just like a common flu or a sinus infection kind of thing."
CD: "So Jennifer, what did you see that really alarmed you?"
Jennifer Hussung: "I think the symptoms started to change after about nine days. I just started to see, like, his energy level change. The fever was more consistent, but the thing that definitely was a trigger for me, I heard about the sense of loss of taste that kicked in. And then he just started kind of seeming like he was breathing a little more winded to me. And then, that's when it quickly changed because then it went to, 'I'm having trouble breathing, take me to the hospital.'"
CD: "So, you take him to the hospital, and how long after you took him to the hospital was he on a ventilator?"
JH: "He was on a ventilator within 24 hours. I dropped him off at noonish, and he spent a day in the hospital, and then, he was transferred to Eskenazi. And within that 24 hours, he went from being on oxygen to three liters of oxygen, to six liters, and then quickly to have a ventilator."
CD: "So emotionally, Jennifer, what are you going through at this time?"
JH: "Completely just worrying, not knowing what was going on, literally being handed a business card that says 'we're calling you, you have to leave.' And that was the most fearful moment for me — just not knowing where he was going to be what was going to happen. So, the first few hours before I got a phone call from headwear, very, very just uncertain nothings — [that is] the best word to describe it."
CD: "How difficult was it for you to know that you couldn't be by his side?"
JH: "That is by far the most difficult thing in this entire situation. It was awful. Luckily, at Eskenazi, where Bryan spent 13 of the 14 days of his hospitalization, they had a great team there. They called it the supportive care team. There was a doctor that was just assigned to me. She wasn't a practicing doctor as far as taking care of patients. She was more of the primary source of communication for families, and she was a lifeline to me because she was my only communicator. Her phone calls were golden to me — they were my lifeline to Bryan."
CD: "So, Bryan, was it fear going through you, or did you say to yourself, 'I've got to be strong for my family?'"
BH: "Right before I got intubated, I had no fear. I knew that I was a Christian. I knew that if it didn't turn out well, I knew where I was going to go, and I knew that my family, they were taken care of, and there was love for me and love for them. Obviously moved to see my family again, but I absolutely had no fear."
CD: "What was the darkest time for you?"
BH: "There was a lot of the dark time. I had some bad memories from when I was on the vent, places that I don't want anybody to have to remember. Just from medication, that was hard. I spent a lot of time alone in my ICU room. Nurses and doctors, they only came in to check on you, so you have no communication, you have no nobody to talk to, and it’s tough. It’s lonely."
CD: "Describe what it feels like to be on that ventilator."
JH: "He doesn't remember any of that because I showed him videos since then and pictures, and he's like 'nope, don't remember that.'"
BH: "Obviously, you can still tell him my voice now. My voice is still recovering from the tubes taken out. I still have to eat really, really slow, and that's a challenge. I’m still eating the softer foods because my jaw is really hurting, and it's just, yeah, I mean it's just a daily struggle."
JH: "Because some of the health care workers were kind enough to take time to take Bryan's phone and call me just for me to see him. So, I know that he was responsive to them because, at one point, I did tell him you know that I loved him and I was, you know, as close to him as I could be through the phone. He gave me a thumbs up once. And once he smiled. I remember the first time that I saw [him] on the ventilator. I was talking to him, and he just kept blinking his eyes over and over and over, and he was kind of mouthing up and down. In my heart, I was like 'oh he's, you know, telling me he loves me and he's OK.' But he doesn't really remember that, unfortunately."
CD: "Was there any point, Jennifer, where you were preparing for the worst?"
JH: "I actually had a very scary moment myself. I, as well, developed some symptoms. I would say that fear factor definitely went into high gear on about Day 4 for us. And I had to kind of make a plan without Bryan here, like, unfortunately we hadn't really talked about that much before this happened, and I just limited with, like, who I could send the the girls to. Their grandparents wouldn’t be nice. So, I called his brother [and said] 'I’m getting symptoms.' That's when the fear factor really went into high gear for daughters of 17 and 14, and it really went into high gear for them to worry that I as well was going to be in the hospital on a ventilator, so I called his brother. And he said, 'the girls are coming here, no questions asked, we’re family, send them here.' So, yeah, there was a very scary day for me. I remember being very afraid that day, just thinking 'oh my gosh, this is happening to me too.'"
CD: "Before you went on the ventilator, it was tough for you to breathe. Describe that feeling of trying to gasp for breath."
BH: "It felt like I had a weight on my chest. I would try to breathe and try to inhale. It was hard. I would inhale, like, I would take air in, but my body wasn’t taking the air. So, it was like trying to breathe in a vacuum chamber. When you try to breathe in and breathe in oxygen, you think you're breathing, but your body's not really receiving the oxygen."
CD: "When did you start seeing the light at the end of the tunnel?"
BH: "You know, the small things — you can stand up from your bed by yourself. And it's a date of rejoice. Small little baby step victories really kept you going."
CD: "Was there a phone call that you got that you knew that you were out of the woods?"
JH: "Yes, actually there was. I had a call every morning and every night. I called one morning, and I could just tell in the nurse's voice. She was just like, 'Oh he's doing great!' You could just here it their tone, like, their progression and how he was doing that they were just genuinely excited for him. And, you know, they were like 'today's going to be a great day, and I do have to tell you that on Palm Sunday.' That's the day that I knew we had turned the corner. It was a big surprise, and our two daughters were asleep and when they come downstairs, and I was like, 'they’re taking the tube out today, and we didn't know, so, and he did great with that.'"
CD: "So, your neighborhood gave you a parade when you came home?"
JH: "We’ve always has a close-knit neighborhood. I just got a message from one of our neighbors. She said, 'I want to do a welcome home parade for Bryan, while social distancing of course.' So, that was really hard for me to keep from him because I knew he was just so excited about coming home and very emotional, it's been a very emotional experience. He got a great send-off at the hospital. The nurses clapped and cheered, and they played 'We Are the Champions.' By the time he got out, he was in tears, so I knew it was going to be an emotional experience in our neighborhood. They really love on us and so they pulled it together and it was probably one of the greatest memories we will ever share together."
CD: "I see the smile on your face, Bryan. How surprised were you?"
BH: "I was very surprised. I mean, that’s love. You know, these people over-stated out there, it's kind of windy, it's kind of chilly, but anytime somebody loves on you, it feels good."
CD: "Jennifer, you mentioned the emotions. What was the most emotional time for you?"
JH: "I think it was from our girls. They really wrestled with the publicity of their dad having this virus. I think it was because, unfortunately, it comes with kind of a fear factor of stigma, you know, just worrying about him and just see all the things that come out of it, so I had to really support them a lot. That was hard to do it alone, but God gave me the strength to do it and for them not to see the breakdowns, and I did have breakdowns, but God really helped me through it and the girls. They love their daddy so much — just seeing their dad home was what they wanted. More than graduation, more than eighth grade dances. But definitely, the girls were the hardest part, to be honest with you."
CD: "Bryan, does this put things in perspective for you?"
BH: "Of course. I mean, it's hard for me to take Jenny's really good notes. Over the past however long it's been, I've started reading some of them — trying to understand what they went through. I was asleep. I was in the hospital, by myself. So, I was dealing with my own problems. I didn't know what they were going through. I'm still learning, I'm still learning, what they were going through, what they were dealing with."
CD: "When you saw that parade that was waiting for you when you're driving through the neighborhood, and you're waving at your neighbors — what were you thinking?"
BH: "I just, I couldn't explain it. I just wanted to cry. I just want people to do nice things for you. People made signs! And they had noise makers and balloons. They didn’t just come out of their house and wave and go back inside. They prepared for this, which was exciting because it's like, man, they actually put forth some effort, and I know that they love us."
CD: "So how does it make you feel when you see people not practicing social distancing?"
BH: "I think they’re crazy."
JH: "That is the one kind of an angry moment I've had through all of this — seeing people not take it seriously when I knew that my husband was in grave danger in the hospital, and I couldn't be there with him. Seeing people saying things and posting things — I don't use that word too often, but it made me very angry."
CD: "So, Bryan, even when you're going through all this, you were still thinking about other people?"
BH: "I did! Actually, Wednesday morning, I wake up, and I'm having trouble sleeping. And I think to myself, you know, why don’t I just order some DoorDash. So, I ordered 50 sandwiches from McDonald’s, and I have it delivered to the hospital for everybody who was working that morning."
JH: "He really wanted a McDonald’s Coke."
CD: "So, you fed McDonald's to the entire hospital?"
JH: "Well, he had to have a Coke!"
BH: "All the employees on my floor. Yeah. I fed them. I was like, I’m feeling good. I don't need all this special help that I did when I first went in there. Why can't I do something nice for somebody who's been there for me and saved my life? I can order them a breakfast. That's what I can do."