Far from 'back to normal': Go inside the ICU as Indiana frontline medical workers continue the fight against COVID-19
13News got a rare look at what life and work is like for frontline health care workers as the coronavirus pandemic continues to hospitalize and kill Hoosiers.

More than a year and half into the COVID-19 pandemic, life has almost returned to normal for many of us.
Students are back in the classroom, sports fans are once again in the stands and people are planning holiday parties.
But one step inside the intensive care unit at your local hospital will show you why doctors and nurses are still more than just concerned about this virus.
They are, as one nurse put it, terrified.
13News got a rare, eye-opening look at what life is really like for our frontline health care workers and what they’re still facing.
“This is an actual look into what it's like,” said Molly Warren, a nurse inside the intensive care unit at Community Hospital South. “I cried a couple of times at work yesterday, and I cried all the way home.”
That’s because, more than 18 months after COVID-19 first appeared, it continues to dominate the ICU at Community Hospital South.
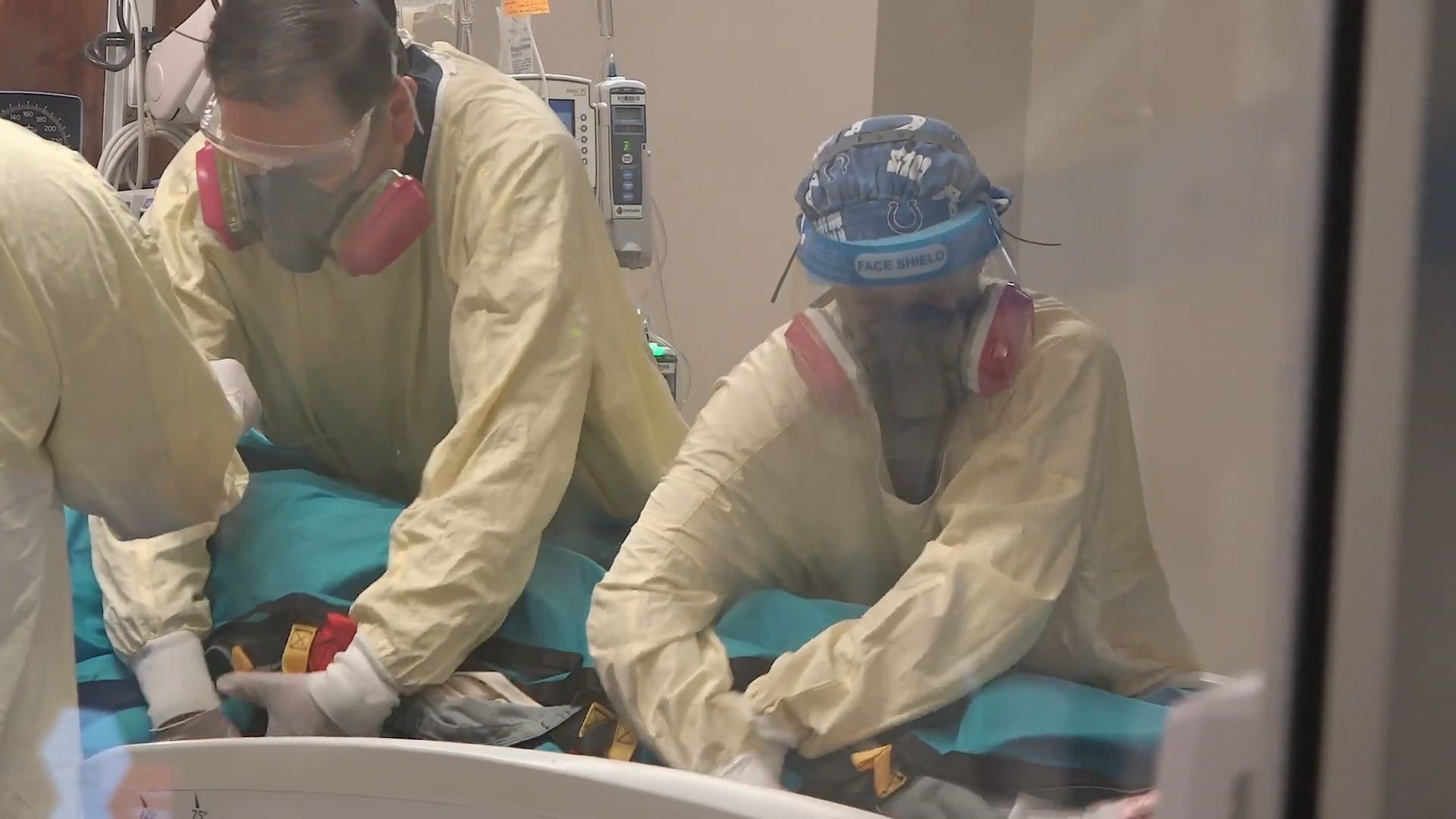
Community Health provided 13News with video that was taken over the span of about eight hours one day earlier this fall.
Inside the ICU

In the Community Hospital South ICU, 11 of the 12 beds were full.
Eight of those 11 patients were COVID-positive. That means they were in isolation — where visitors were not allowed.
One man was struggling to breathe and wanted to call his wife.
“This is Laurie, your husband’s nurse today,” said the nurse into the phone. “We're at that point we're gonna have to put him on a ventilator — a breathing machine — because we're having trouble oxygenating him. So he wanted to call and tell you he loves you before we sedate him.”
Due to patient confidentiality, 13News wasn’t able to find out what happened to that particular patient.
"Unfortunately, this is a conversation we have to have way too often,” said Erin Willis. “I’ve held more hands of people dying in the last year and a half than anyone should have to in a lifetime. Sometimes, I get mad and just want to throw things because it is frustrating — day after day.”
Because those patients are in isolation, Willis said nurses aren’t just providing medical care for them. They play a variety of crucial roles.
“They can’t have a family member in there with them. They’re alone,” said Willis. “So we’re playing nurse, family member, loved one, chaplain sometimes, dietary doctor. I mean, we play all the roles.”
Some patients in the unit on this particular day were well enough to be moved to other units within the hospital.
The problem was, there were no beds available.
So, those patients remained in the ICU.


“It’s just — that’s life now. We’re on diversion. Every hospital in the city is on diversion,” said Willis.
Diversion means ambulances have to find another hospital to take incoming patients. But when every hospital is on diversion, Willis said they can’t refuse patients. Someone has to treat them.
So hospitals find a place — any place — to put them so they can be cared for.
It can be a tricky problem. One that, according to nurses, every hospital in Indianapolis was facing that day.
'We're Exhausted'
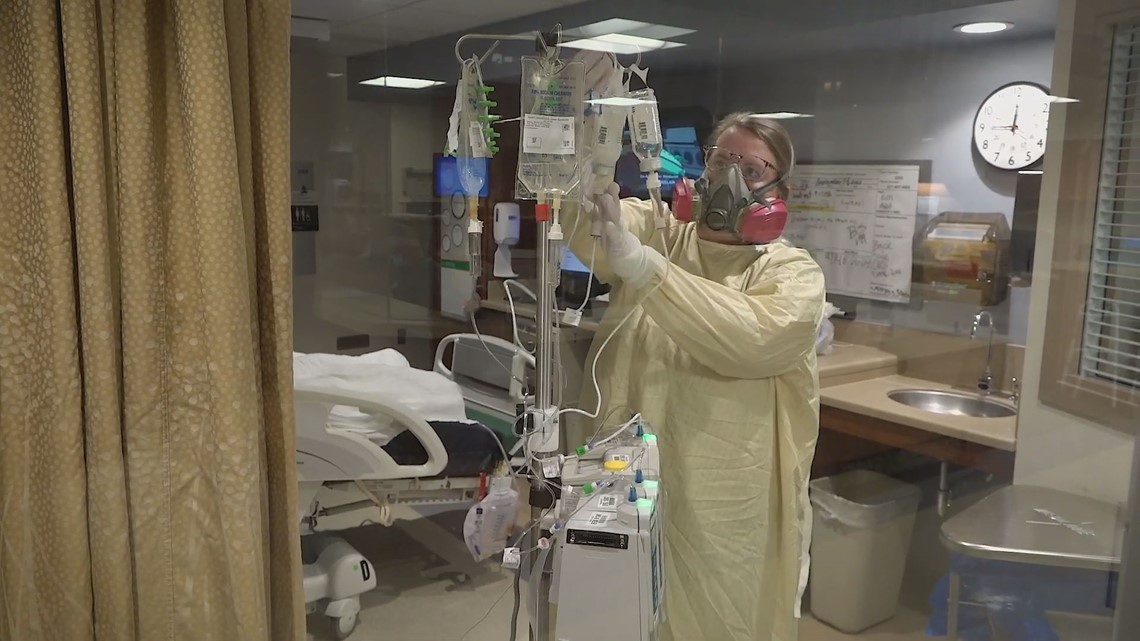
“We're exhausted. Just exhausted,” said Marcus Guajardo, ICU nurse manager at Community Hospital South. “We are fighting as hard as we can, but it is getting harder and harder to keep that fight up.”
The intensive care unit of a hospital has always been home to life and death struggles. But Guajardo said this is different.
“This surge and the last surges we’ve had ever since the vaccine has come out has made things 10 times worse only because we have solution,” he said. “We still have half the country choosing not to do it [get vaccinated], and it's very frustrating.”
ICU nurses said none of the COVID-19 patients in the ICU at that time had been vaccinated.
“Usually, our country comes together at some of our worse times. But I feel like right now we are a divided country, and I wish science wasn’t politicized. I don’t care if you’re a Republican or a Democrat or who you voted for,” Guajardo said. “What matters is — we can end this death and all of this illness if we come together as a country and get vaccinated.”
Guajardo said managers today are focusing more than ever on emotional assistance programs for their employees. They're also encouraging frontline workers to take time off.
“As nurses, we learn, we adapt we make it work and continue to come back everyday to take care of our patients,” said Willis.

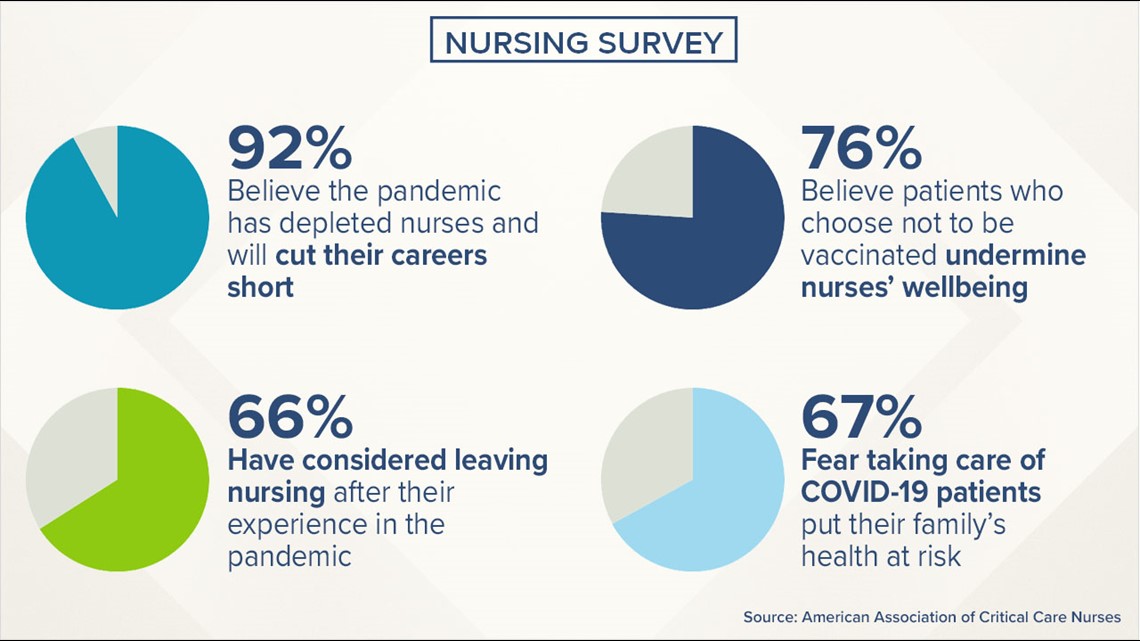
But not all nurses feel that way anymore. According to a survey for the American Association of Critical Care Nurses, 66% of respondents said they felt their pandemic experiences have led them to consider leaving nursing. Nine in 10 said they think the pandemic has depleted nurses at their hospitals, and because of this, their careers will be shorter than they planned.
Guajardo heard from one of those nurses.
“She told me she has seen too much death — that she loves being a nurse, loves being in health care, but had to do something else because of all the death that she's seen over the last year and a half,” he said.
Impact at Home

Guajardo says frontline health care workers can’t leave their pandemic work at work.
"I lie in bed at night just thinking about what the next day's going to bring,” he said. "I know this has taken an emotional toll in myself, and I can't imagine what its done to my staff."
When Willis comes home, her husband, Brent, can see the toll it’s taking.
"I definitely see it wearing on her and way more than I used to. And to see that to the people who you love and care about the most — is terrible,” said Brent.
“There’ve been multiple time during this that I’ve said ‘How do we get you out of there?’ But I know that’s her passion that’s what she loves to do.”
They offer what only they can — their love and support.
“It’s a huge help because I think if I did not have that, I would be in a much worse place,” said Willis.