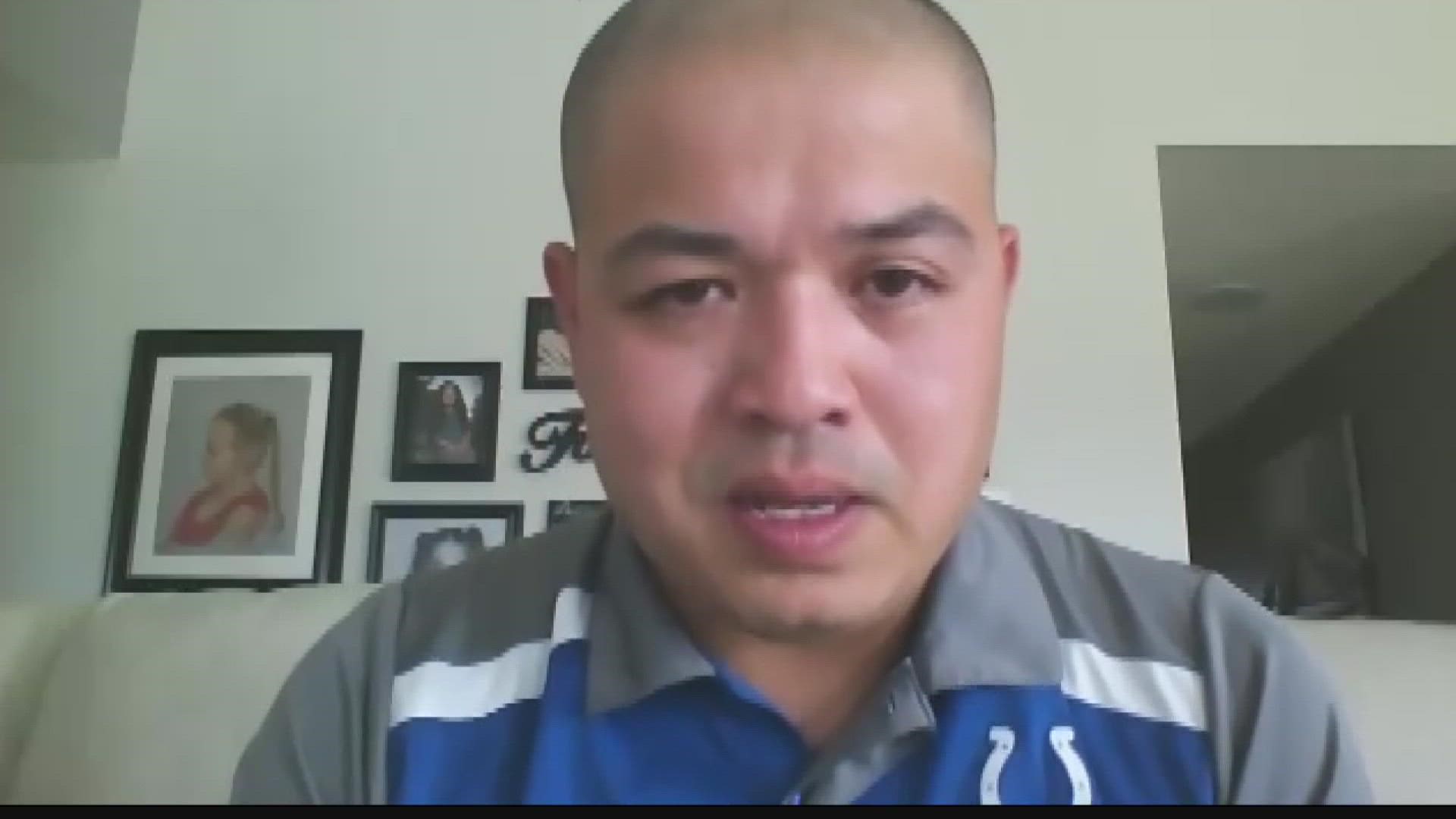
INDIANAPOLIS — Twenty-two percent of nurses said they may leave their current position, according to a recent survey by McKinsey. Shane Myint has been an emergency room nurse for 13 years and said the health care profession has never seen anything like this pandemic before.
Myint said he intends to stay in nursing because he loves where he works and he loves helping people. But he admits it's not easy, and he's had to take steps to prioritize and protect his mental health.
Hitting a wall
Myint knows firsthand how strong-minded nurses are, but the pandemic is a breaking point.
"I've been a nurse for 13 years and it's getting difficult to keep that good spirit going," Mynt said. "Nurses have hit a big wall. There’s been a national shortage of nurses who are leaving the workforce because of the pandemic. It's really hard to take care of patients every day when you are running eight or nine nurses short every shift."
Myint said at his hospital, they can't move patients to some beds because there aren't enough nurses to care for them. Sometimes, that puts a burden on the ER nurses.
It's a reality many experts have been warning of during the pandemic. The U.S. health care infrastructure does not have the capacity to care for a large influx of people into the hospitals at one time, while also caring for the day-to-day emergencies and long-term illnesses.
"It's emotionally and mentally draining for us," Myint said.
Mental health is health
Myint said he has had the opportunity to pick up more hours with the staff shortage, but he chose not to for his own mental health.
"I'm trying to keep myself sane," Myint said.
COVID-19 patients typically need around-the-clock care.
"They are very time consuming. You have to do many things to make sure this patient doesn't go south," Myint said.
But it's not just the toll of caring for ill patients causing stress. It's the false hope of getting past the pandemic.
"We thought we won and now we're in a third wave," Myint said. "This is the hardest thing we've ever been through. Never in our lifetimes have we been through something like this."
Most frontline workers will agree that the physical part pales in comparison to the mental challenge of working in the pandemic. And as a result, many will agree that PTSD is rampant among frontline workers.
Some nurses are retiring early or transitioning to travel assignments where they can make at least double what they do as a staff nurse. Others are switching to outpatient. Myint said from his health care colleagues across the country, he can think of 10 that have either retired or transitioned to a different type of nursing position.
Myint, who has type 2 diabetes, said he tries to keep active to cope. He started running marathons and tries to get health care workers together to play in sports and just have fun and unwind away from the hospital.
He said staying active and having a wife who is also a frontline worker has helped him cope with the fear and trauma.
"I'm deathly afraid of bringing this stuff home to my children, to my mother who's ill, to my spouse, my friends," Myint said. "Spreading this to my immediate family — that's what I'm afraid of."


Myint noted that in the last few months as the delta variant surges, even young, healthy people — primarily the unvaccinated — are getting infected, which scares him.
"There's 50% of the population walking around unvaccinated without masks, that’s what scares me the most," Myint said.
'Anything is better than nothing'
Myint said it's rare to see someone who has been vaccinated in the ER with COVID-19.
"If they do get sick, it's very mild to moderate symptoms, not moderate to severe symptoms," Myint said. "Most of the patients on the ventilators are predominately unvaccinated individuals."
Myint said he has some friends who have lost friends and family members overseas because they didn't have access to the vaccine.
"My father currently lives in Burma," Myint said. There, they only have access to a vaccine manufactured by a Chinese state firm. "He personally asked me if he should take it, and I said 'anything is better than nothing.'"
The reality is that many in the United States who are ending up in the ER critically ill from COVID-19, aren't there because they medically can't get the vaccine or didn't have access to it, but because they choose not to get vaccinated.
"It is very disheartening — to a point that sometimes makes you angry — because I 100% blame this third wave on the unvaccinated," Myint said. "We're all nurses. We're all medical professionals. We all have to take care of those who are sick. I just genuinely feel disappointed for them who don't take a vaccine that is available to them."
This time, frontline workers said they're better prepared for this third wave than they were for the first two.
"For a while, we were reusing our N95 because there was a shortage," Myint said. "Now that we have plenty of supply, we are able to get a mask basically for every patient that we have."
Myint said he's continuing to go to battle, and as a frontline worker, he asks that people support their fight.
"When patients say 'thank you for all that you do' but turn around and know that they're unvaccinated, are they really thanking me for all that I'm doing? Or are they just doing the opposite of what I'm sacrificing for?"